By Chelsea Yates
When it comes to cardiac systems research, Patrick Boyle wants to play his cards right.
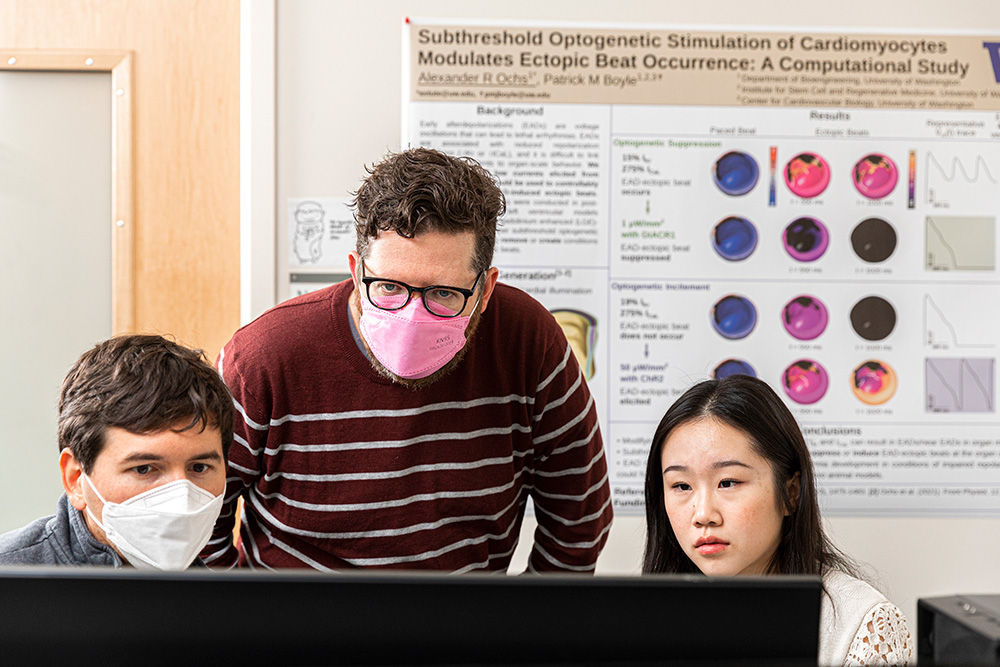
Patrick Boyle, center, with bioengineering Ph.D. candidate Alexander Ochs, left, and junior Jamie Yang, right, in the CardSS Lab. Photo by Mark Stone / University of Washington
Growing up, the assistant professor of bioengineering loved playing cards with his family and named his UW research laboratory — the Cardiac Systems Simulation (CardSS) Lab — in part to honor the pastime. But a more surprising connection between family and research was still to come.
“I don't know how many people in my line of work have the opportunity for their research to manifest in front of their eyes, in a loved one no less,” Boyle says. “It’s been surreal and humbling.”
In the CardSS Lab, Boyle’s team models heart rhythm disorders to help doctors better understand and predict when patients may be at risk of arrhythmia, cardiac arrest and stroke. Central to their work is atrial fibrillation (A-fib), a type of arrhythmia that’s very common — the Centers for Disease Control and Prevention (CDC) estimates that 12.1 million people in the U.S. will have A-fib by 2030 — yet difficult to detect.

“I don't know how many people in my line of work have the opportunity for their research to manifest in front of their eyes, in a loved one no less. It’s been surreal and humbling.”
“It’s tricky to diagnose because in many cases A-fib can occur spontaneously without any sign something might be amiss,” Boyle explains. “Some people have persistent episodes and are well aware of their condition, but for others it comes and goes. Episodes of A-fib can cause shortness of breath or palpitations, but many folks have no symptoms whatsoever, which makes those occurrences especially challenging to catch.”
With monitoring and treatment, people with A-fib can live regular lives. Left untreated, it can increase a person’s risk of stroke. During an episode, the heart's upper chambers beat irregularly and out of sync with the lower chambers, which can lead to blood clots in the heart. According to the CDC, A-fib is the cause of one in seven strokes, yet many people don’t discover they have A-fib until something significant like a stroke occurs.
For years, Boyle has been working to draw more attention to the correlation between A-fib and stroke and improving A-fib screening and treatment using cutting-edge bioengineering tools and techniques.
Even so, he wasn’t prepared when, last September, his dad experienced what would be the first of two strokes — and a perspective shift on his own research was in the cards.
Two strokes in five days

Boyle with his dad, Mike Boyle. Courtesy of the Boyle family
Boyle was preparing to travel out of the country when he received a call about his dad. His parents had been driving from their home in Calgary to Seattle when Boyle’s father lost the peripheral vision on his right side.
“Somewhere between Spokane and Seattle, he’d had a stroke, but we didn’t realize that yet,” Boyle says. “His symptoms were minimal. Honestly Dad seemed more annoyed about the whole thing.”
After his dad sought medical care in Seattle, the team quickly confirmed a stroke. Following an overnight stay and several diagnostic tests, he was discharged on a dual antiplatelet therapy (DAPT) course of treatment to prevent an unwanted clot. After a few days of rest, Boyle and his brother drove their parents home.
About an hour from Calgary, Boyle’s father unexpectedly suffered another stroke, this one much more serious than the first. This time the symptoms were on his left side — a sign that this stroke was affecting different territory in his brain than the first one. An ambulance rushed him to the hospital, where he had a blood clot removed from his brain via an endovascular thrombectomy (EVT) procedure.
Within an hour Boyle’s father seemed nearly back to normal and able to move his left side with surprisingly few limitations.
“His pre- and post-EVT scores on the NIH stroke scale were 14 and 3. That scale goes from 0 to 42. If what I saw in Dad was a 14, I never need to see anything above that,” Boyle says.
A surprising discovery
Due to capacity issues in the stroke recovery unit, medical staff kept Boyle’s father in the emergency department, which would prove important. On Boyle’s watch, a few days later, his dad’s ECG heart monitor started flashing “AFIB.”
“He didn’t have a known history of A-fib, and there had been no physical change,” Boyle says. “I notified a nurse, who called in the electrocardiography team to confirm that he was definitely in A-fib.”
They could see on the heart monitor that his heart rate had abruptly increased by about fifty percent, but he felt nothing different. “This is a message my lab and I have been sharing for years — A-fib is insidious because people can be in it but have no idea — and here it was, right in front of me, happening to my dad,” Boyle says.

Boyle and bioengineering Ph.D. candidate Savannah Bifulco examine heart rhythm disorder simulations in a computational model derived from the MRI scans of a stroke patient. Photo by Mark Stone
It’s also possibly why Boyle’s father experienced two very different strokes in five days. During A-fib, blood clots created near the heart can be released. Depending on their size and if they make their way to the brain, they can cause a stroke, which is what doctors believe happened during the second stroke. While there was no clinical documentation of arrhythmia from the hospital in Seattle, Boyle believes the evidence points in that direction.
In a way, the discovery was uncanny. “Had he been transferred out of the emergency department, the nurses told me they likely wouldn’t have had him on an ECG because other units don’t routinely monitor the heart, and so we likely wouldn’t have known he was experiencing an episode at all,” Boyle says.
‘A renewed vigor’
Adjusting to life with a heart condition, Boyle’s father is now on an anticoagulant to minimize the stroke risk. He’s been using his smartphone to track his heart rhythm since he doesn’t feel different during an episode. Boyle says his dad has tracked about eight, each lasting anywhere from one to eight hours. Activities such as meditation and walking have helped him come out of an episode.
For Boyle, the experience has brought a major shift in his approach to research and teaching.
“Dad’s episode was precisely the kind of ESUS (Embolic Stroke of Undetermined Source) that motivates a large part our lab's work,” he says. “Imagine if we had better tools to help decide whether someone who's had a stroke like Dad's first one should be sent home on DAPT or if it's warranted to use a stronger drug like an anticoagulant earlier on, despite the increased risk.”
Boyle is encouraging his students to broaden their view.
“We need to ask different questions and figure out better ways to bring our research to the bedside,” he says.
A big part of this is expanding collaborations between physicians and engineers. At the UW, Boyle works closely with Dr. Nazem Akoum, a cardiac electrophysiologist who directs the atrial fibrillation program at UW Medicine, to use data from A-fib patients’ MRI scans to run simulations that can inform new treatment strategies. He also works with Juan Carlos del Álamo, a professor of mechanical engineering who specializes in cardiac biomechanics and fluid dynamics, to study connections between disease-related changes to heart tissue, rhythm disturbances and clot formation.
“The deep partnership between medicine and engineering drew me to the UW in 2018,” Boyle says. “That doesn’t exist everywhere, but it’s critical to making an impact.”
Above all, he feels a reawakened commitment to his work. “As long as I’ve studied this stuff, I’ve never had the chance to observe someone who’s having an episode of A-fib,” he says. “There’s a lot of complex work ahead, but I feel a renewed vigor to help solve problems and advance heart health.”
In the meantime, he’s looking forward to enjoying more card games with his dad.

Boyle plays cribbage with his father and son, Clare. Courtesy of the Boyle family
Engineering and heart health
The Cardiac Systems Simulation (CardSS) Lab uses MRI scans, computer models and other tools to learn more about heart rhythm disorders and to develop new treatment strategies.
Author’s note: I lost my dad in 2008 to a stroke. Though that was 15 years ago, not a day goes by that I don’t think about him. My dad had a history of heart disease that I don't know much about. In fact, just last month — while working on this story — I learned that my dad lived with A-fib. I’m thankful to Pat and his father for trusting me to help tell their story, and I’m grateful to the many researchers like Pat and his team who are working every day to better understand, treat and prevent heart disease and stroke.
Originally published March 13, 2023