Engineering heart health
By: Ed Kromer
A collaborative cohort of UW Engineering researchers is helping unlock the mysteries of the human heart at the Institute for Stem Cell and Regenerative Medicine.
Jennifer Davis was an early career kinesiologist looking to expand her understanding of muscle physiology in a biomechanics lab when she first encountered a human heart cell. Unlike other living muscle cells that appear static under a microscope, a heart cell pulses. Visibly. Rhythmically. A microscopic microcosm of the beating heart itself.
For Davis, it was love at first sight.
“That’s what I’m going to work on,” she decided on the spot.
Now an associate professor of bioengineering and pathology and interim director of the UW Institute for Stem Cell and Regenerative Medicine (ISCRM), Davis has dedicated her career to reversing an endemic malady of those pulsating heart cells that first captivated her.
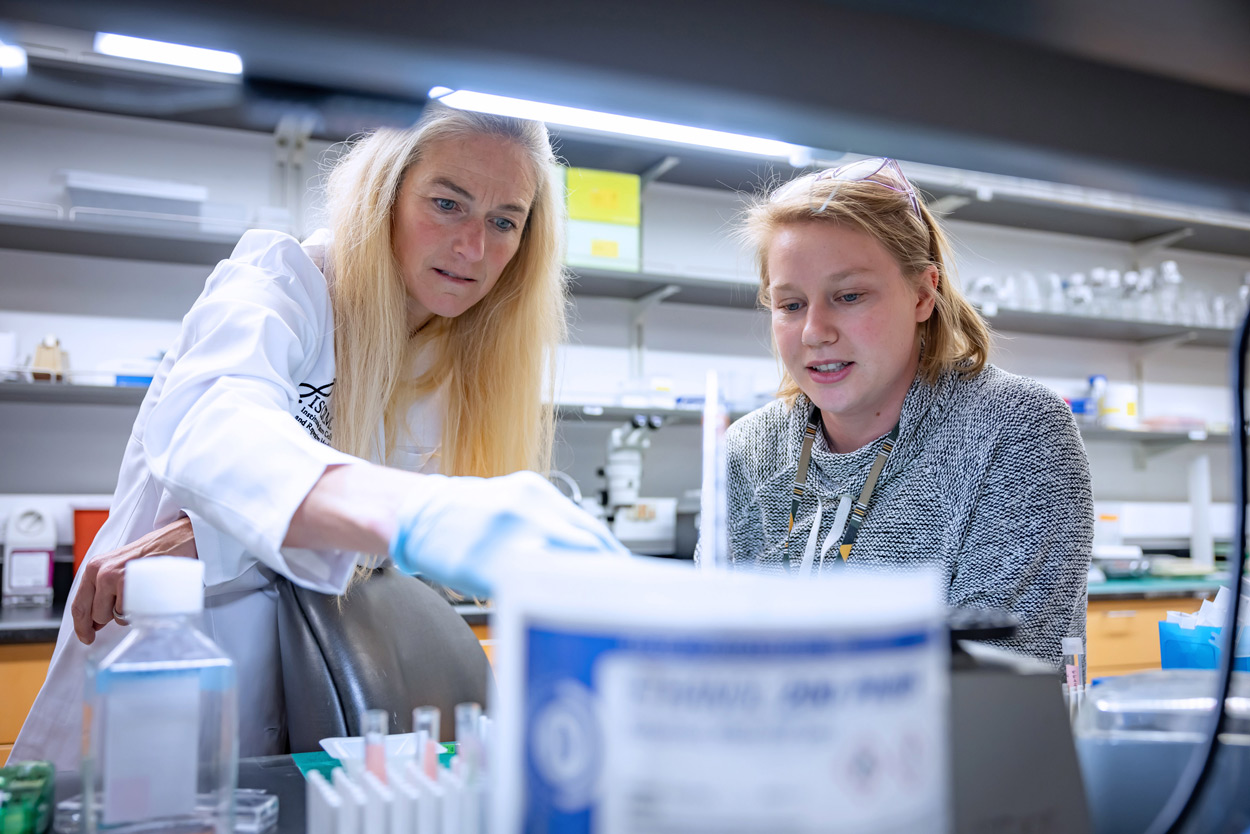
In her lab, Jennifer Davis, left, designs tissue to improve cardiac function. Institute for Stem Cell and Regenerative Medicine
She’s in good company at UW Medicine’s sprawling ISCRM (colloquially pronounced “ice cream”). This multidisciplinary convocation of researchers from around the world — organized into 150 interwoven labs representing 40 departments in the School of Medicine, the College of Engineering and several others — is advancing stem cell biology and regenerative medicine to enhance the human body’s astonishing power to heal itself.
Like Davis, many of those researchers have been drawn to the cardiovascular system. It’s not hard to see why. The human heart is the core of our very being, metaphorically and physiologically. A muscle of exquisitely complex architecture and profound importance, there are still myriad mysteries to its function and dysfunction.
And to an engineer, a good mystery is irresistible.
“Engineering is a problem-solving discipline,” says Nathan Sniadecki, a professor of mechanical engineering and the institute’s interim co-director. “And the heart presents a wide array of problems.”
At ISCRM, Davis, Sniadecki and a collaborative cohort of UW Engineering and UW Medicine researchers are approaching the heart from multiple angles and with multiple technologies, some repurposed and others newly invented.
What can mend a broken heart?
Davis’s research focuses on scarring, or fibrosis. As elsewhere in the body, damaged heart cells get replaced by scars. But unlike other parts of the body, “the heart doesn’t repair very well,” she says. “It’s a bad general contractor.”
The buildup of scarring can inhibit the normal functioning of the heart and lead to its failure.
So, the Davis Lab has worked for more than a decade to discover how to reverse scarification through a “remodeling process” that uses cell and tissue engineering.
“We know the cell type responsible for making the scar,” Davis says, “and some of the molecules in that cell that, if you turn them on or off, will change the way in which they make the scar.”
Her ultimate goal is to develop a “designer scar” that would improve cardiac function on its own but also optimize the host environment for integrating therapies that replace lost or damaged muscle into the heart and synthetically regenerating it to full function. This would revolutionize treatment of heart disease.
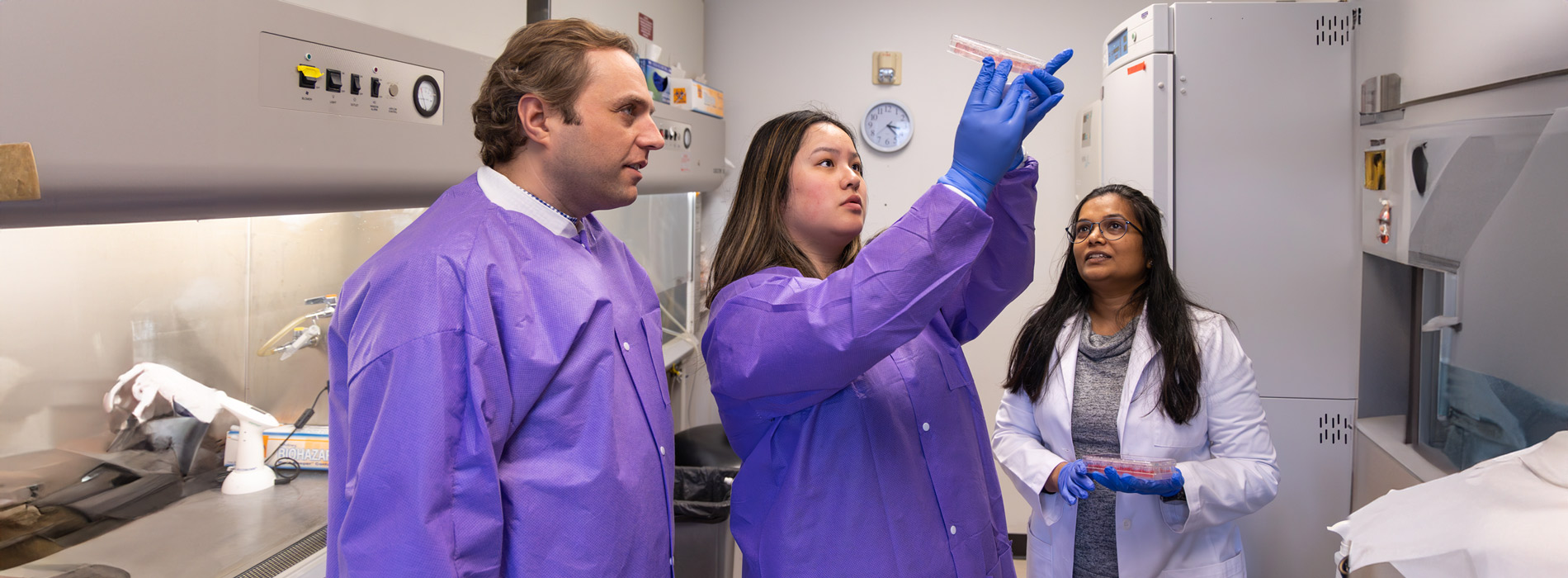
Nate Sniadecki, left, examines tissue specimens with researchers. UW Medicine
Measuring heart hardiness
Sniadecki approaches the heart from a biomechanical perspective, designing and developing tools, at micro and nano scales, that measure the resilience of heart cells against the forces weighing against them.
“The heart is a very complex system with so many confounding factors,” he says. “So, how do you reduce the variables?”
His Cell Biomechanics Lab embeds these tiny measurement tools in engineered myocardial tissue to create insightful testbeds for the human heart — outside the human heart. “Now you have cells in a three-dimensional environment that are working together like real tissue from real human biology performing real functions,” Sniadecki says.
This enables cause-and-effect biological examinations that would be exceedingly difficult to do inside a real human body. These testbeds have been applied to calculate the effects on the heart of common and experimental drugs and therapies, genetic defects, aging — even prolonged time in space.
Sniadecki hopes the work of his lab will construct a more efficient bridge between basic science and clinical application.
When sparks flicker
While Sniadecki is concerned with the mechanical nature of the heart, Patrick Boyle explores the electrical. A professor of bioengineering with a background in electrical and computer engineering, Boyle applies computational tools and techniques to investigate the systemic consequences of arrhythmias — electrical abnormalities of the heart.

Patrick Boyle applies computational tools and techniques to investigate arrhythmias. University of Washington
His Cardiac Systems Simulation Lab models rhythmic disorders to help doctors better understand and predict when patients may be at risk of conditions like atrial fibrillation (Afib), cardiac arrest and stroke, which can strike without warning (in fact, Afib struck his own father without warning in 2022).
Recently, Boyle has begun applying artificial intelligence and machine learning to enhance the power of predictive modeling. New projects are harnessing massive repositories of patient data — millions of UW Cardiology electrocardiogram readings to better understand the risk of sudden cardiac arrest and thousands of Fred Hutch Cancer Center echocardiograms to calculate the risk of heart disease for childhood cancer survivors.
“We’re looking for warning signs in the data, trying to pick up on features that are below the threshold of human visual perception,” Boyle says. “This is machine learning for good.”
On the other side of these enhanced prediction methods is the promise of more calibrated forms of treatment.
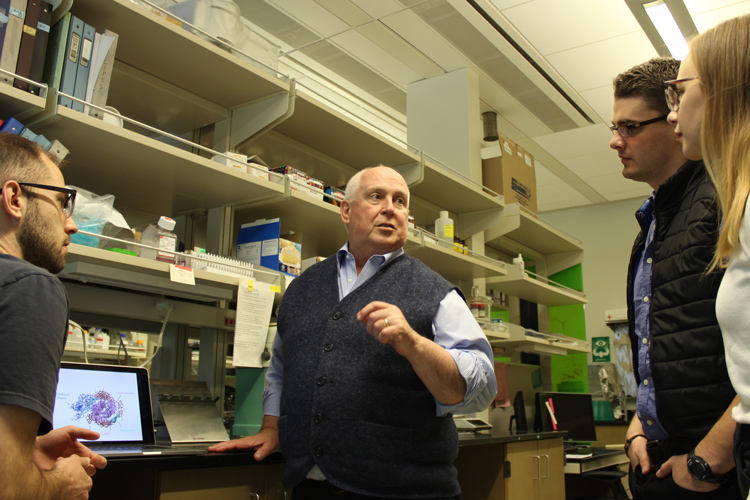
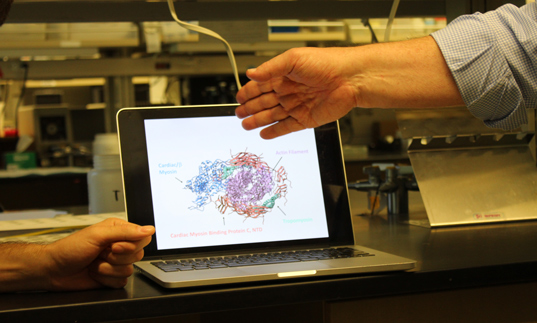
In the Heart and Muscle Mechanics Lab, led by Michael Regnier (main image, center), researchers use a combination of experimental and computational techniques to examine the entire scaffolding of cardiac architecture. UW Medicine
Whole heart solutions
Michael Regnier, a professor of bioengineering, takes a multiscale approach to heart dysfunction resulting from genetic disorders, natural trauma, aging and comorbidities such as obesity and diabetes.
His Heart and Muscle Mechanics Lab uses a combination of experimental and computational techniques — developed in-house — to examine the entire scaffolding of cardiac architecture, from microscopic proteins interacting at the cellular level all the way to that prodigious hunk of meat that regulates the circulation of blood throughout the body.
In genetic heart disease, Regnier says, “the site of insult precipitates ‘pathological remodeling.’ A lot of structures end up being affected to compensate for the change that’s happening at the molecular scale.”
But the process can be reversed. A recent Regnier lab study mapped how a minute engineered change to the composition of myosin, the heart’s molecular motor, triggers a positive chain reaction from cell to tissue to organ, ultimately strengthening heart function and reversing heart failure.
From this discovery, Regnier and his colleagues are working on an effective therapeutic for patients. “Eventually,” he says, “the treatment we develop could become part of the heart failure management regimen.”
Engineers bring the tools

A researcher in the Cell Biomechanics Lab handles tissue samples. UW Medicine
Many more UW Engineering faculty contribute to heart research at ISCRM, by designing synthetic cardiovascular environments and applying fluid dynamic, protein design, 3D bioprinting and many more approaches.
The secret to their collective advancements in engineering heart health is not only the brilliance of individual researchers and labs, but also the comprehensive and collaborative culture of the institute they work in — and the UW at large.
“The environment is truly multidisciplinary and highly collaborative,” says Regnier. “It’s a powerful model that allows us to cross-pollinate our research programs and our trainees, too.”
They collaborate with researchers across ISCRM and the neighboring Center for Cardiovascular Biology and Center for Translational Muscle Research. And they frequently partner with UW Medicine clinicians such as Dr. Farid Moussavi-Harami, a cardiologist who honed his research skills in the Regnier lab, and who brings valuable patient insights.
“Having each component of the heart within the same center allows an exchange of ideas to holistically understand how the heart functions both in health and in disease,” Davis says.
In this institute of biomedical discovery, UW engineers are contributing an essential skill set and innovative perspective. They are adapting ideas and technologies from existing fields — and inventing new ones all the time.
“We only know the planets and stars because we were able to build telescopes. We’re only able to study cells because we built microscopes,” Sniadecki adds.
Engineers are inventing new tools that lead to new understanding of the human heart. Biology asks the questions and engineers find a way to answer those questions.”

Engineering excellence for the public good
We are committed to creating a healthier and more just world through our work.